
New Targets for Treating Dermatological Diseases Discovered by SoBT Researchers
Chronic pruritus, or itch lasting longer than 6 weeks, is a debilitating and surprisingly widespread affliction. Generally originating in the skin, chronic pruritus is extremely common in patients suffering with dermatologic disorders, such as eczema and psoriasis. It is also associated with a multitude of systemic, neurologic and even psychiatric disorders, with primary disease ranging from renal insufficiency to multiple sclerosis. Perhaps not surprising when you consider its diverse etiology, chronic pruritus affects a massive percentage of the population. Current estimates put the lifetime prevalence at 22%, meaning that more than 1 in 5 people will experience chronic pruritus at some point in their life.
Beyond the physical damage and scarring, patients with chronic pruritus often face disturbed sleep, impaired focus, and even mental health disorders like depression and anxiety. Unfortunately for sufferers, current anti-itch treatments are ineffective or are associated with significant side effects. Though unacceptable, this reality is understandable when we consider the history of itch research.
Traditionally, itch was classified as a submodality of pain, with little known about its specific mechanisms and features until the first itch-specific receptor and neural pathway were discovered. Since then, scientists have worked to map out normal itch circuits and to understand how this system is altered in chronic pruritus. Though the last decade has brought great advances in basic itch research, much remains unexplored and clinical options remain scarce.
One group in the School of Biotechnology, led by Dr. Jianghui Meng and Dr. Jiafu Wang, has been attempting to address this issue by examining the mechanisms of cellular communication, examining the link between epidermal skin cells and the nervous system in conditions of chronic dermatological pruritus. A recent publication from the group outlines the role of a transient receptor potential, or TRP, ion channel in pruritic skin disease and highlights a novel neuro-epidermal pathway involved in sensitisation of this important TRP receptor.
‘Improving the understanding of the underlying signaling networks is an essential step in the development of new and effective anti-itch therapies’, explains Ciara Larkin; lead author on the recently published article. ‘Ion channels are pore-forming membrane proteins which facilitate rapid changes in cell activity and act as key coordinators of cell-to-cell communication and one particularly interesting group of ion channels is the TRP superfamily, which act to integrate and coordinate sensory responses, including both pain and itch. Until recently, itch research largely centred on two specific TRP channels, namely TRPV1 and TRPA1. These channels are found on sensory neurons, where they respond to itch-inducers and coordinate neural itch circuits’.
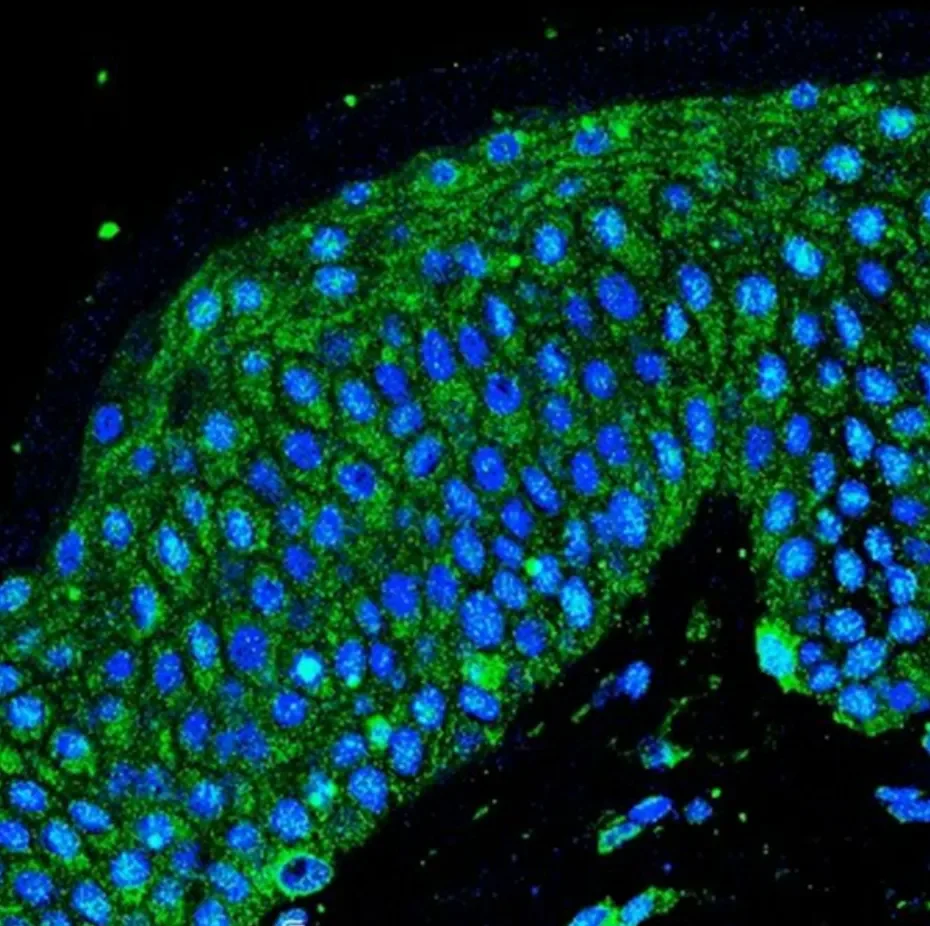
‘This project focused on a different member of the TRP family, namely TRP vanilloid channel 3 (TRPV3). The TRPV3 channel is highly expressed in the epidermal layer of the skin and has been linked to both acute itch and pruritic skin conditions. Despite this, the pathways underpinning the function and dysfunction of TRPV3 remain elusive’.
‘We hoped to gain a better understanding of TRPV3 activity, signaling and sensitisation, and to examine what role, if any, these pathways played in itch processing and clinical dermatitis’.
‘This work was carried out with scientists from the International Centre for Translational Neuroscience in Henan University; with Prof. Andrea Szegedi and her group in the University of Debrecen Medical School in Hungary; with Prof. Timo Buhl from the University Medical Centre Göttingen in Germany; and was supported by Dr. Dermot Walls and Dr. Sandra O’Neill from the School of Biotechnology. Together, we examined murine models of acute and prolonged itch, primary skin cultures, and samples from patients with eczema and psoriasis. This multi-tiered approach was especially important to us and allowed us to maximise the translational importance of our findings’.
‘Thanks to our donors, we were able to show that TRPV3 is increased in human eczema and psoriasis, compared with healthy skin, and that the increase is specific to the lesional areas. This suggests that TRPV3 expression is correlated with disease severity or lesion stage’.
‘Previous work from our group showed that IL-31, a known itch-inducer and cytokine common to dermatitis, can promote the release of B-type natriuretic peptide or BNP from itch neurons. We wondered whether this neuropeptide could affect the epidermal TRPV3 channel. Using cultures of epidermal skin cells, we found that BNP both increased TRPV3 transcripts and sensitised TRPV3 activity’.
‘We then looked to characterise the signaling pathways acting downstream of the TRPV3 channel. These experiments linked TRPV3 activation to the release of Serpin E1. We had never heard of Serpin E1 but when we examined our eczema samples, there it was; Serpin E1 was highly and specifically increased in the lesional eczema. Thanks to the incredible work by Ms. Weiwei Chen, the joint first author on this paper, we now know that Serpin E1 also represents a potent itch-inducer in both acute and prolonged murine models’.
‘This paper outlines the clinical importance of TRPV3 and TRPV3-targeting drugs in chronic pruritic dermatitis. Together with previous findings, our work revealed novel neuro-epidermal and itch-inducing pathways, highlighting several targets for future anti-dermatitis and anti-itch agents. Ultimately, this research could prove hugely beneficial for the millions afflicted by chronic pruritus in the world today’.
For more information, the group’s latest article can be found here.
