
“Anxiety, grief, fear, isolation and distress for residents, families and staff” highlighted in study on the impact of COVID-19 on residential care homes
A new study on the impact of COVID-19 on residents, their family members and staff of residential care homes, led by Dr Mary Rose Sweeney from Dublin City University’s School of Nursing, Psychotherapy and Community Health, has found that the pandemic had significant adverse effects for residents, family members and staff in residential care settings for older people in Ireland.
Isolation, loss of connectedness as well as a reduction in the level/quality of care provision led to significant physical, psychological and social impacts for both residents and their families. Staff reported high levels of stress, trauma and burnout. Family input to care was suspended, with adverse consequences.
Key Findings
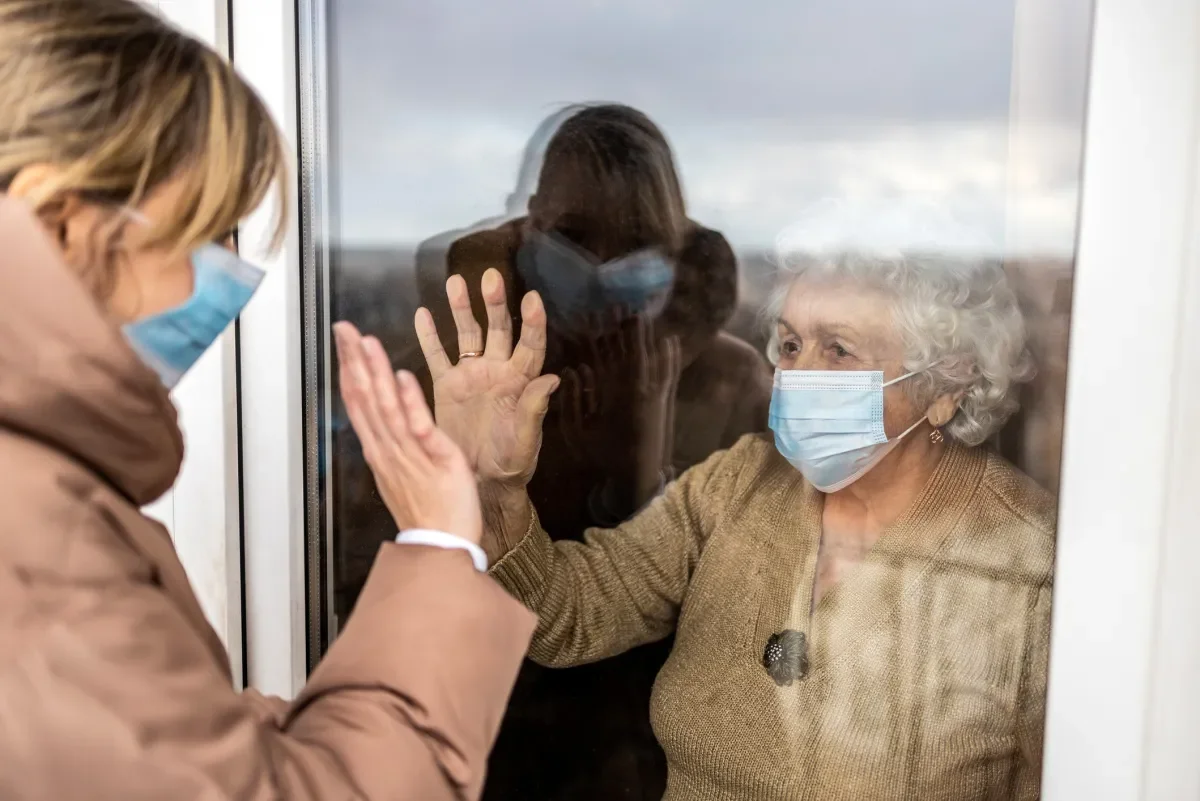
- Family members experienced fear, distress, anxiety, loneliness, helplessness, frustration and some participants experienced physical challenges such as being outside in all weathers trying to communicate via a window.
- Families described an acute decline in their loved one’s physical health which included weight loss, reduced mobility, pressure sores, dehydration, and unkempt appearances, which some found shocking and distressing during the pandemic.
- The majority of families did not perceive themselves to be visitors, but regarded themselves as continuing in their caregiver role in the residential environment.
- Staff reported that at least one third of residents were confined to their own room without company during the first wave of the pandemic.
- Staff observed many adverse psychosocial impacts for residents and families, the most significant issue being that they were unable to see their loved ones during the pandemic, resulting in loneliness and loss of connection.
- Staff experienced high levels of stress and burnout, followed by concerns about virus transmission, trauma, fear about death of residents and self.
Other significant findings
Mental health/social health
- 98% of residents could connect remotely with their family members during the pandemic.
- High level of remote connectedness was deemed to be of poor quality and unreliable by many family participants in the qualitative interviews.
Physical health
- Usual care of patients who did not contract COVID-19 was reduced or neglected during the pandemic.
Rates of infection
- Some respondents felt that years of under-investment in state facilities had led to residents sharing bedrooms and this combined with poorly ventilated common areas contributed to/facilitated viral spread.
- The transfer of infected patients from the acute hospital sector and movement of staff across different sites resulted in increased virus spread.
- A high proportion of staff and family carers believed that the rate of infection could have been reduced by more effective/diligent infection control measures.
- Family members believed that residents who did not have family members to advocate for them were at higher risk during the pandemic.
Impacts on staff
- The personal toll on staff ranged from information overload, physical and mental exhaustion, supporting their peers and covering for colleagues while off sick, in addition to managing their own fears.
- The majority of staff had put the needs of residents above their own needs.
- Many staff expressed their distress at witnessing the impact of the virus on vulnerable people who were traumatised, alone and fearful.
- Staff were angry and distressed about the numbers of care staff who contracted the virus and felt unsupported and that their well-being and safety had not been valued or protected.
- Multiple issues relating to staffing were highlighted, including low staff-to-patient ratios, due to staff shortages arising from self-isolating, illness and redeployment. Other issues of concern included high turnovers, too few senior staff, staff who lacked the specific skills required, as well as too many agency staff.
Role of the media
- While media reports were regarded as important in highlighting the issues in residential care in relation to the rapid viral spread and the need for prompt intervention, some staff and families were distressed at the level of media blaming.
- Headlines of failures and fatalities caused distress to residents and families and made some staff feel ashamed and embarrassed by where they worked.
Recommendations
- Residential care management needs to ensure that visiting restrictions are balanced with the rights and needs of residents.
- The important supplemental caregiving role of family members needs to be recognised, valued and supported by management and staff.
- All sites should facilitate access to one designated family member who would visit residents on an ongoing basis even in the event of a pandemic
- Mandatory staff skill mix requirements and staff-to-patient ratios should be agreed at national level and implemented at local level by residential care management and staff.
- Residential care managers should proactively work on strategies to enhance the retention of their staff and reduce their reliance on agency staff.
- Managers need to advocate for, and introduce adequate psychological support, debriefing and practice supervision systems for staff urgently.
- Residential care settings should upgrade their IT infrastructure and upskills staff, residents (where appropriate) and family members.
- Holistic patient centred and ethical decision making is essential at all times.
- Specialist infection control programmes for those working in residential care settings should be developed and made mandatory training for all staff.
- Agreed national principles and minimum standards should be implemented for improving governance/management, infrastructure /facilities and access to GP and other allied health professionals.
Speaking about the study, Dr. Mary Rose Sweeney, Head of the School of Nursing, Psychotherapy and Community Health, said
“Our study shows that COVID-19 caused much anxiety, grief, fear, isolation and distress for residents, families and staff and highlighted the important role that family members have in residential care settings for older people.
In future communicable disease outbreaks, the needs and rights of residents to see loved ones should be balanced with the public health imperative.
In addition to mental health impacts, the deterioration of residents’ physical health was a strong finding, with family participants expressing shock and distress at this rapid decline. Some of this deterioration may have been COVID-19 related but in many cases it resulted from the reduction or absence of usual care. Our study highlights the extent to which family members had hitherto provided direct care, and the importance of this to their loved ones.
The loss of the caregiving role was a major source of distress to family members particularly when they observed the mental and physical deterioration of their loved ones which arose from them being prevented from providing care.”
The study was conducted by a team of academic researchers at the School of Nursing, Psychotherapy and Community Health which included Dr Mary Rose Sweeney, Dr Ciara White, Dr Mary Nevin, Dr Andrew Boilson, Dr Briege Casey and Prof Anthony Staines and Mr Patrick Boylan from the School of Psychology.
A two-phased mixed methods study was conducted, consisting firstly of an online survey administered to staff, residents and family members, with follow-up interviews with family members. The researchers opted for an anonymous survey so that staff could freely provide answers without fear of being identified. The survey sent to residents and family members was also anonymous with an option to be contacted for a follow up one-to-one interview.
The full report is available here.
